
Investigation How Air Pollution Triggers Immune Imbalance and Lung Damage
Chronic exposure to PM2.5 and PM10 activates oxidative stress and NRF2, driving allergy-like lung inflammation
Long-term exposure to particulate matter (PM) can disrupt immune balance and worsen lung health. In a recent study, researchers from Korea exposed mice to PM10 and PM2.5 to examine their effects on lung inflammation and immune responses. The results showed elevated TH2 cytokines and activation of the NRF2 pathway, contributing to allergic-type lung damage. These findings suggest that air pollution may promote asthma and chronic lung diseases by altering immune regulation and increasing oxidative stress.
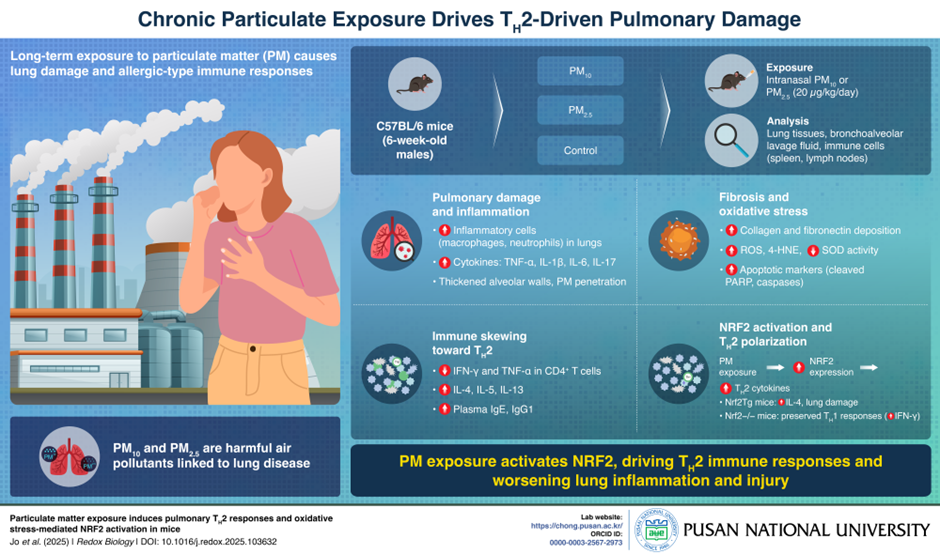
Image title: How Air Pollution Triggers Allergic Lung Inflammation
Image caption: Long-term exposure to PM2.5 and PM10 triggers oxidative stress and activates the NRF2 pathway, shifting the immune response toward TH2 inflammation—worsening asthma and other allergic lung diseases.
Image credit: Professor Changwan Hong from Pusan National University, Korea
License type: Original Content
Usage restrictions: Cannot be reused without permission
Air pollution is a global health concern, with over 90% of the world’s population breathing air that exceeds World Health Organization safety standards. Fine and coarse particulate matter are especially dangerous, as they can penetrate deep into the lungs and bloodstream. While the link between air pollution and respiratory diseases is well established, how these pollutants disrupt immune responses in the lungs has remained unclear.
In a recent study, a team of researchers led by Professor Changwan Hong from Pusan National University School of Medicine, South Korea, investigated how long-term exposure to particulate matter triggers immune imbalance in the lungs. “Our study reveals how chronic exposure to particulate matter (PM10 and PM2.5) triggers harmful allergic-like (TH2) immune responses in the lungs by activating oxidative stress and the NRF2 pathway,” explains Prof. Hong. This paper was made available online on 8 April 2025 and was published in Volume 82 of Redox Biology on 1 May 2025.
Using a mouse model, the researchers exposed mice to PM10 and PM2.5 daily for 16 weeks. They then analysed lung tissue, plasma, and immune cell profiles to evaluate how particulate matter affected lung health and immune function. Mice exposed to PM showed significant signs of lung inflammation, including alveolar wall thickening, immune cell infiltration, and tissue scarring. These effects were more severe in the group exposed to PM2.5, which is known to reach deeper areas of the lungs.
The researchers also observed a marked shift in immune response. TH1-type immune activity, associated with protective responses, was suppressed, while TH2-associated signals increased. This included elevated levels of cytokines such as IL-4, IL-5, and IL-13, and higher levels of IgE and IgG1, antibodies linked to asthma and allergic inflammation. These findings suggest that long-term exposure to PM skews immune balance toward an allergic-type response.
This immune shift was closely linked to activation of the NRF2 pathway, a key regulator of oxidative stress. NRF2 typically protects against environmental damage, but under chronic activation, it appeared to worsen inflammation. “This mechanistic link explains why air pollution can worsen asthma and other allergic diseases, identifying NRF2 as a key driver of this shift,” Prof. Hong notes.
The study offers insight into how chronic air pollution affects respiratory health at a molecular level. By linking NRF2 activation to immune reprogramming, the findings highlight new potential therapeutic targets, such as antioxidants or drugs that regulate NRF2 activity.
“Our findings suggest that targeting oxidative stress or modulating NRF2 activity could be a new strategy to treat or prevent pollution-induced allergic inflammation, such as asthma,” says Prof. Hong.
Overall, the research provides a clearer understanding of how pollution impacts the immune system and supports the need for stronger air quality regulations to protect vulnerable populations.
Reference
Title of original paper: Particulate matter exposure induces pulmonary TH2 responses and oxidative stress-mediated NRF2 activation in mice
Journal: Redox Biology
DOI: 10.1016/j.redox.2025.103632
About the author
Prof. Changwan Hong is a Professor of Anatomy and Vice Dean of Research at Pusan National University School of Medicine in South Korea. His group focuses on immune regulation, cytokine, T cell immunity and CAR-T immunotherapy. Prof. Hong earned his PhD in immunology from Korea University in 2007 and received postdoctoral training in cellular immunology at the NIH and Stanford University. An expert in T cell development and cytokine biology, he has authored numerous scientific publications and is dedicated to translating immunological research into improved public health outcomes.
Lab:
ORCID ID:
0000-0003-2567-2973
 PURCS_168_Infographic_final.png
(2MB)
PURCS_168_Infographic_final.png
(2MB)